
For most patients these resolve within weeks however, high alveolar dead space in ∼30% of recovered patients suggests persistent pulmonary vascular pathology.Ĭhew MS, Blixt PJ, Ahman R, et al. We speculate impaired pulmonary gas exchange in early COVID-19 pneumonitis arises from two concurrent, independent and variable processes (alveolar filling and pulmonary vascular obstruction). Shunt was marginally elevated for two patients however, five patients (30%) had elevated alveolar dead space. Both shunt (% cardiac output) at 10.4% (0-22.0%) and alveolar dead space (% tidal volume) at 14.9% (0-32.3%) were elevated (normal: <5% and <10%, respectively), but not correlated (p=0.27).

Arterial blood (breathing ambient air) was collected while exhaled oxygen and carbon dioxide concentrations were measured, yielding alveolar-arterial differences for each gas ( P A-aO 2 and P a-ACO 2, respectively) from which shunt and alveolar dead space were computed.įor acute COVID-19 patients, group mean (range) for P A-aO 2 was 41.4 (-3.5-69.3) mmHg and for P a-ACO 2 was 6.0 (-2.3-13.4) mmHg. We studied 30 patients (22 males mean±sd age 49.9☑3.5 years) 3-15 days from symptom onset and again during recovery, 55☑0 days later (n=17). We aimed to measure shunt and alveolar dead space in moderate COVID-19 during acute illness and recovery. We propose that measuring respiratory gas exchange enables detection and quantification of these abnormalities.
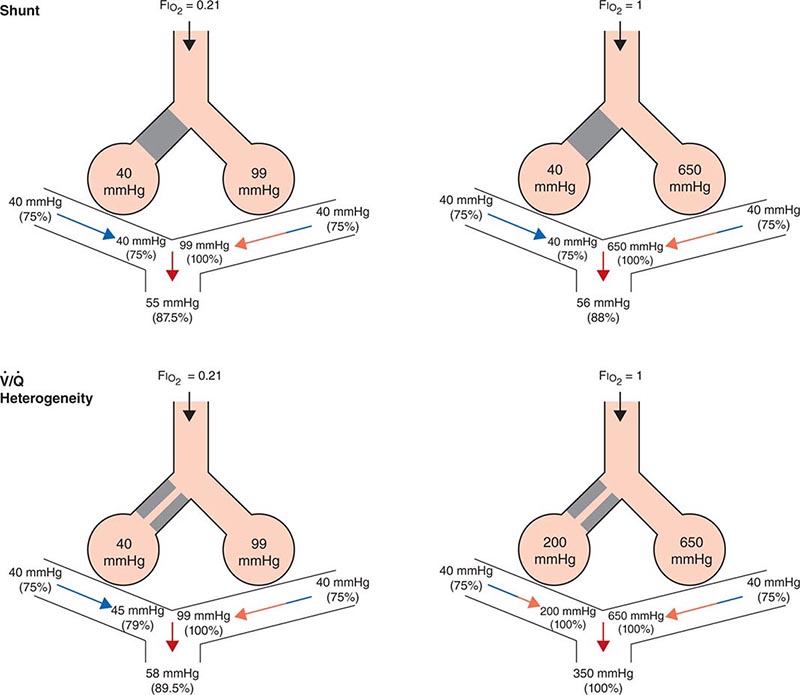
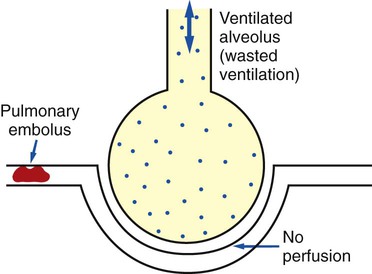
Pathological evidence suggests that coronavirus disease 2019 (COVID-19) pulmonary infection involves both alveolar damage (causing shunt) and diffuse microvascular thrombus formation (causing alveolar dead space).


 0 kommentar(er)
0 kommentar(er)
